The use of skilled nursing facilities as short and long term post-acute care settings has become very prevalent. At the moment, there are nearly 16,000 certified skilled nursing facilities in the U.S and the number keeps rising.
Why is this happening?
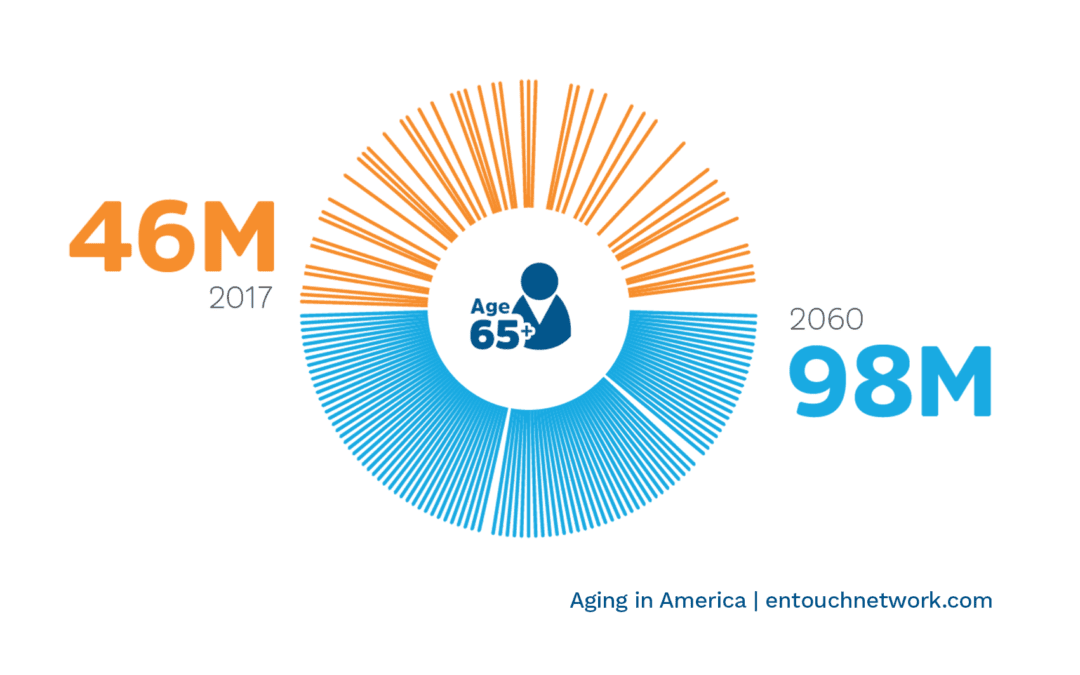
The number of adults aged over 65 years is rapidly increasing and is expected to double its current population of over 46 million to 98 million by the year 2060.
This means that more and more seniors are requiring skilled nursing services, and in order to meet this rapidly growing need, more skilled nursing facilities are opening and expanding. Simply put, there are (and will continue to be for the foreseeable future) more adults whose short term and long term medical and personal care needs have to be catered for by trained professionals.
Another major factor that has contributed to their growth is the decision of Centers for Medicare & Medicaid Services (CMS) to penalize hospitals that have high readmission rates. Transferring patients to skilled nursing facilities to recover helps hospitals lower their readmission rates and therefore keep financially afloat.
What are Skilled Nursing Facilities?
These are facilities that, in addition to regular nursing home services, offer skilled and professional medical care to seniors. They are most times used as a recovery/rehabilitation center for seniors who just completed a hospital stay and still require medical care. For instance, after undergoing procedures like hip replacement surgeries, most seniors will still need advanced medical resources and skills to perfect their recovery before they go home. Skilled nursing facilities dispense with the need for them to remain in the hospital, while still allowing them to have access to needed medical care, along with other personal care services. Skilled nursing care is often used for diabetic rehabilitation, wound care, stroke recovery, respiratory care and general illness recovery.
Skilled nursing facilities offer both short and long term services. For many seniors, stays at skilled nursing facilities are merely temporary. They are used as an interim point of care for recovery after a hospitalization due to an illness/injury. For others whose medical needs are constant and permanent, such as those suffering from chronic diseases, long-term stays at skilled nursing facilities are the norm.
Some of the professionals and workers at skilled nursing facilities are Physicians, Registered Nurses (RNs), Registered Dietitians (RDs), Certified Nursing Assistants (CNAs) Licensed Practical Nurses (LPNs), Physical Therapists and Speech-Language Pathologists.
How Do They Differ From Traditional Nursing Homes?
Aside from the fact that skilled nursing facilities provide medical care and nursing homes do not, there are other important distinctions between them.
Skilled nursing facilities are strictly regulated by the Centers for Medicare & Medicaid Services (CMS) and the U.S Department for Health. They are certified by the government and must adhere to stringent regulations and requirements in order to maintain their certifications. This close supervision is mainly because they offer medical services which require a certain level of training and expertise. Nursing homes, on the other hand, are not as closely monitored because they offer only custodial and non-medical services. However, they get surveys and inspections by state agencies, and these are used to assess patient satisfaction.
Skilled nursing facility care is covered by Medicare and Medicaid (in some instances) while the costs of staying in a traditional nursing home are generally out of pocket. However, due to the growing need, some nursing homes now offer skilled nursing and medical short-term services too.
Medicare and Skilled Nursing Facilities
Skilled nursing care is covered under Medicare Part A (Hospital Insurance). It covers skilled nursing care provided in skilled nursing facilities for a limited time and under some conditions. Summarily, patients with Medicare are covered if they have completed at least 3 days of inpatient hospital stay and their doctors determine that they need daily skilled care from skilled nurses or therapy staff. Additionally, this patient must enter the skilled nursing facility within 30 days of leaving the hospital and it must be a facility that’s certified by Medicare.
For Medicare patients transferred to skilled nursing facilities by (currently 514) hospitals participating in the Bundled Payments for Care Improvement (BPCI) initiative Model 2, the 3-day inpatient stay requirement is waived.
Payment and Costs
The Bundling and Coordinating Post-Acute Care Act of 2015 applies to skilled nursing facilities. How it works is that post-acute care (PAC) coordinators in hospitals establish networks of post-acute care providers like skilled nursing facilities. The coordinators and their networks of PAC providers will then manage patient’s care for either 30, 60 or 90 days, using a fixed amount of reimbursement (target amount). The time starts on the day of the person’s discharge from the hospital and continues till the last day in the skilled nursing facility. If the patient has to be readmitted into the hospital, the PAC coordinators will be held accountable for the cost, but participants (coordinator, provider and hospital) will be rewarded if the total cost of a patient’s care is lower than the patient’s bundled payment (target) amount.
How Dina can help
Dina assists with making the transition from hospital to skilled nursing care go smoothly by allowing post-acute care coordinators to search for and accept referrals digitally. It also sends real time updates on patients’ conditions and enables these coordinators to pinpoint the right time to move them to skilled nursing facilities and eventually back to their homes. Dina ultimately closes the communication gap between all care givers as a patient transitions from hospital to home.




