Summary
Learn how SDOH data can be used to improve care coordination, while also creating more healthy days at home for patients.
As the cost of healthcare continues to skyrocket, providers are looking for ways to achieve better outcomes and drive down costs. As we work toward a more coordinated approach to care, one question is often missed: How do we create more healthy days at home? CareCentrix‘s Jon Terenzetti, Vice President of Data and Technology Transformation, shares his insights.
In many cases, care defaults to an acute setting, due to an inability to control non-clinical factors, often called social determinants of health (SDOH), like the environment, family, and socio-economic status.
But we know that 80% of health outcomes are determined by what’s happening outside of a doctor’s office. This is why patient risk assessments that focus only on clinical measures, claims and comorbidities often come up short.
SDOH Data is Lost in Translation
While the impact is significant, there often is a disconnect between payers and providers in terms of assessing and measuring social factors. Insurance companies have all the claims; they have the data. They know exactly what’s happening with patients and what they’re doing with their health.
We’ve seen that better data sharing can move the needle on addressing social determinants of health.
Providers know what’s happening on the ground. And that on-the-ground information often gets lost in translation. It doesn’t fit into an EMR; it doesn’t fit into a claim. We’ve seen that better data sharing can move the needle on addressing social determinants of health. This is becoming more important as the healthcare industry understands how to leverage technology to fill a critical care gap between hospitals, providers and patients.
CareCentrix recognizes the importance of data sharing and has engaged Dina, a leader in real-time patient tracking across the care continuum. This partnership is valuable since the Dina platform is able to introduce new data elements at scale to give us a nuanced understanding of patients and their needs inside and outside the home. Armed with this data, we can begin to drive more targeted and cost-effective interventions.
SDOH Data + Action = Change
Data is a representation of something happening in the real world: it is a timestamp or a risk score or an index that relates to how actual events occur. How you use that data to change future events requires action. A key lightbulb moment for me was recognizing that there are some blanket learnings that are easy to put in place and can improve outcomes for a large number of people. For example, in a recent study of over 50,000 CareCentrix patients, we found that:
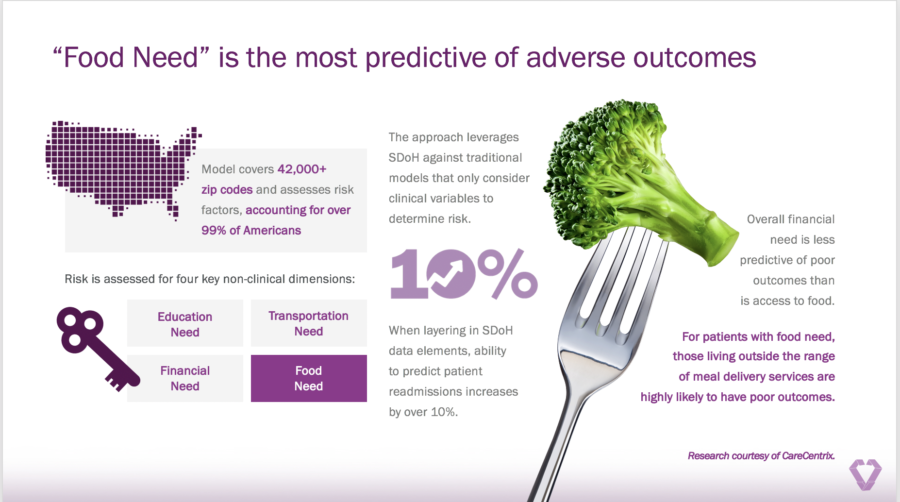
● Food need is the most predictive of adverse health outcomes when measured against education, transportation and financial need.
● Access to food is four times as predictive of adverse health outcomes as financial need.
● Living near a meal delivery provider such as Meals on Wheels decreased the risk of readmission more than any other non-clinical factor.
Therefore, asking questions about food availability, identifying food needs, and then signing up patients for meal delivery services, are some of the easiest things we can do to have the biggest impact. These types of insights allow us to focus resources where we know our interventions will drive improved outcomes.
Dina introduces new SDOH data elements at scale to give us a nuanced understanding of patients and their needs inside and outside the home. Armed with this data, we can begin to drive more targeted and cost-effective interventions.
How to Start? Impact and Ease
While we can’t address every patient’s needs, the glimmer of hope I see is that we can use what we’ve learned to address a large portion of them. Great ideas are rarely executed by starting with the hardest part. I think the real opportunity here is to start addressing the factors that are most important and easiest to impact – driving the greatest potential for improvement.
Access to food and transportation, for example, are easy to impact at scale, with meal delivery or transportation vouchers. Helping people apply for government assistance, or to programs to which they’re entitled, is also scalable and impactful.
We know one of the most impactful measures is housing insecurity. It’s extremely important but very difficult to address. This is an area where you need to build a long- term approach. However, a short-term solution is to assess a patient’s home for safety and accessibility, addressing key issues proactively.
Leaning in for Change
One barrier is that social determinants don’t fit in the traditional confines of what healthcare is supposed to do. And there is a legacy of complexity in the industry that hampers the willingness of people to lean in. We can make a huge impact by taking a few simple steps: raise awareness of social determinant needs, look at the data we have, and begin to think differently about the types of interventions at our disposal and how they can create value. If your goal is to drive the best outcome for patients, focusing on these steps can make a huge, meaningful impact.
By: Jon Terenzetti, Vice President of Data and Technology Transformation at CareCentrix, the leader in home-based and post-acute care (PAC) services.
Interested in hearing how organizations are using technology to improve patient care? Sign up for our newsletter today.