
Seniors, people with disabilities, and those with chronic conditions rely on Medicaid home and community-based services (HCBS) to live independently outside of nursing homes and other institutions.
Medicaid fills an important gap as the sole source of coverage for most HCBS. Medicare, for example, covers a limited amount of skilled post-acute care. Private insurance typically does not cover HCBS, especially to the extent needed by people who rely on those services to meet daily needs, and out-of-pocket costs can be financially prohibitive. Other funders for HCBS might include private long-term care insurance.
HCBS programs are often funded by state waivers, which are part of a state’s Medicaid program, and they provide a special group of services to a certain population. Waivers usually require medical and financial eligibility, and this may not be the same as state Medicaid eligibility.
Who is Using HCBS Waivers?
Nationally, 3 million people receive HCBS through waivers, and over 2.5 million people receive HCBS as part of the state plan benefit package (primarily home health and personal care services).
Joint federal and state Medicaid HCBS spending totaled $116 billion in 2020, with the vast majority (96%) for optional services. Waivers continue to comprise the majority of HCBS spending and the 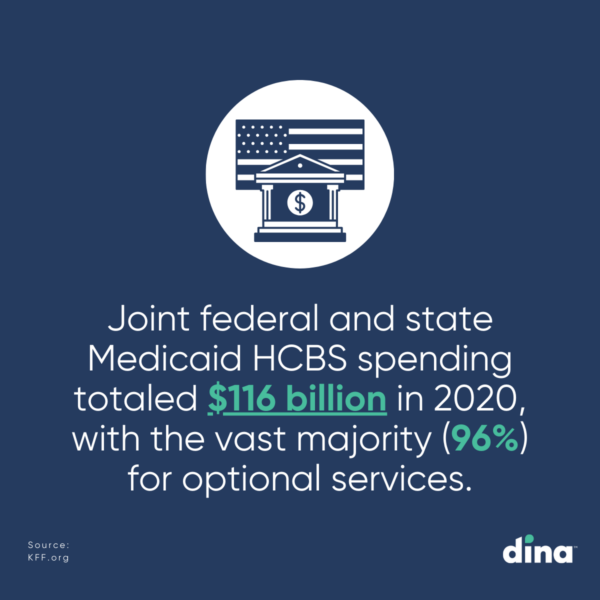
Nationally, there was modest spending growth and modest changes in the number of people receiving HCBS from 2019 to 2020, though some states experienced larger changes. States identified a growing senior population and the pandemic as driving increases in the number of people served and/or spending in HCBS waivers.
Among waiver target populations, spending for people with intellectual and developmental disabilities (I/DD) is disproportionate to the number of people served because per-person costs for this population ($48,900) are higher than per-person costs for seniors and adults with physical disabilities ($17,600).
What are HCBS Waivers?
HCBS waivers became available in 1981 to provide states with a way to provide long-term services and supports (LTSS) outside of institutions. Skilled nursing care and home health services are mandatory services in Medicaid, but because many individuals need additional services to stay in their homes, Medicaid favored institutional care. Families often had to put their loved ones in a nursing home to get them the care they needed.
HCBS waivers gave states a new way to address the LTSS needs of their residents. Using HCBS waivers, states can make people eligible for Medicaid who were previously only financially eligible if they were in a nursing home or other institution. States can also create packages of services specifically designed to keep people in their homes, including home modifications, respite care for family caregivers, and enhanced home health services.
Some people receive services through both waivers and state plan benefits. Most people receiving HCBS get services that are provided at state option, which results in substantial variation among states.
HCBS Waivers Waiting Lists
These waivers also allow states to choose – and limit – how many people are served. States’ ability to cap HCBS waiver enrollment can result in waiting lists when the number of people seeking services exceeds the number of waiver slots available.
Over 707,000 people were on HCBS waiver waiting lists in 40 states in 2017, an increase of 8% over 2016. While this suggests some degree of unmet need for HCBS, waiting list data alone are an incomplete measure of state capacity and demand for HCBS and are not directly comparable across states. The populations served and how they are defined vary among states, and everyone on the waiting list may not be eligible for services.
PACE Members Expect Quick Activation of Home-Based Services.
Does Your Plan Deliver?
See how easy it is to streamline access to medical and non-medical
home-centered benefits, support your centers, and quickly measure results.
What are HCBS?
HCBS programs address the needs of people with functional limitations who need assistance with everyday activities, like getting dressed or bathing. They are often designed to help people to stay in their homes, rather than moving to a facility for care.
HCBS programs fall into two categories: health services and human services. Health services include home health care, durable medical equipment, case management, personal care, and hospice care.
Human services support daily living and can include senior centers, adult daycares, home-delivered meal programs, personal care, transportation, home repairs and modifications, and homemaker services.
HCBS Benefits and Challenges
Creating and maintaining HCBS programs benefit the community and the individuals served in many ways. However, there are several challenges to consider that come along with this type of program.
Some benefits include:
- Cost-effective–usually less than half the cost of residential care
- Meets most people’s desire to age and/or receive care at home
- Some waivers permit family members to be paid caregivers
Some challenges include:
- Long-standing unmet need for home and community-based services among seniors and people with disabilities
- Direct care workforce shortages
- State-level variation in Medicaid eligibility, spending, and services
- Availability of qualified caregivers
- Caregiver burnout
- Access to providers
- Skilled nursing care includes only medical services performed by a registered nurse. Other daily tasks fall primarily to family members
Who Runs HCBS Programs?
Within individual states, HCBS care is provided by lead agencies and other service providers. A lead agency acts as the primary care coordinator for its region—for example, a county’s Department of Human and Social Services. Service providers contract with the lead agency in their area to provide services.
In addition, CMS offers several national programs that can support certain types of HCBS in different communities:
Program of All-Inclusive Care for the Elderly (PACE) combines many services into one comprehensive program and often combines Medicare and Medicaid eligibility.
Money Follows the Person (MFP) Rebalancing Demonstration Grant moves eligible people from nursing facilities back into the community, which helps states rebalance the long-term care systems of their Medicaid programs. The Money Follows the Person-Tribal Initiative (MFP-TI) is a special initiative under this program that is currently available in five states. It helps tribes in those states more easily provide home- and community-based services and move members from facilities back to their communities.
Medicaid fills an important gap in the spectrum of healthcare coverage options available today. It is often the only source of many HCBS that seniors, people with disabilities, and those with chronic conditions rely on to live independently.
States would be more likely to increase the number of people receiving waiver services (which can be capped) if more federal funds without an expiration date were available. The new funding would help states improve the HCBS delivery infrastructure and expand services to fill existing and anticipated unmet needs.
Understanding current state-level variation in Medicaid eligibility, spending, and services for seniors and people with disabilities is important to inform upcoming policy debates.
Members Expect Quick Activation of Behavioral Health Services. Does Your Plan Deliver?
In under 2 minutes, we’ll show you how easy it is to coordinate behavioral health and home-centered benefits to your members and quickly measure results.




