
CMS has signaled a renewed commitment to health equity with the introduction of the Health Equity Index (HEI), designed to motivate Medicare Advantage (MA) plans to identify and address disparities in care to members with social risk factors such as dual-eligibility, low-income, and disabled populations.
The new HEI reward provides a unique opportunity for Medicare Advantage organizations to review their health equity strategies and align with the latest and upcoming legislative requirements. The CMS 2024 Final Rule provides a framework to help plans prepare.
“I think we can all agree that CMS’s strategy to promote health equity and address social determinants of health is long overdue,” said Dina CEO Ashish V. Shah. “It’s great to see some policy focus around it.”
His advice to health plan leaders: prioritize health equity, embrace technology, and improve the member experience.
What is Health Equity?
Until now, there has been much talk about the need to remove the factors that hinder equitable health care access and delivery. To clarify its intent, CMS defined health equity as the attainment of the highest level of health for all people, where everyone has a fair and just opportunity to attain their optimal health regardless of race, ethnicity, disability, sexual orientation, gender identity, socioeconomic status, geography, preferred language, or other factors that affect access to care and health outcomes.
What is the Health Equity Index?
One of the biggest opportunities to advance health equity is with the newly established Health Equity Index Reward (HEI reward) for the Star Ratings system.
The HEI will replace the existing reward factor for earning Quality Bonus Payment (QBP) incentives. To earn rewards, MA organizations will need to focus on identifying populations with social risk factors and deploying interventions to eliminate barriers to care. The HEI reward is intended to encourage both Medicare Advantage Part C and Part D plans to improve care for members.
Populations Covered by the Health Equity Index
- Members with disabilities
- Members who qualify for low-income subsidies
- Members who qualify for dual Medicare and Medicaid eligibility
In the future, CMS may consider including other at-risk populations such as members with a specific area deprivation index, a measure of a neighborhood socioeconomic landscape that factors in income, education, employment, and housing quality.
Health Equity Index Benefits and Implications
The HEI provides a framework for CMS to create standards for data collection, and Medicare health plans to collect health equity data systematically. This is crucial to identify where disparities exist. And, it can help focus the resources and interventions necessary to address disparities, measure progress, and hold health plans accountable to providing quality care for everyone.
The HEI will also empower people to choose plans that provide excellent care since the score could eventually be included in the Medicare plan finder.
Health Equity Index Challenges
Establishing the HEI will help all parties understand and address many healthcare disparities. Still, several issues may pose a challenge to the creation and use of this new measure.
First is incomplete data reporting. One of the issues is that the CMS programs don’t collect all health equity data, due to limited authority and enrollees sometimes opting out of voluntary reported data.
The index will first focus on specific at-risk populations. But there are still many other groups of people who experience health inequities but won’t be included in the initial HEI assessments because of a lack of data. For example, the CMS doesn’t collect SDoH data such as income.
Another challenge is that there’s currently no health equity data standard. For Medicare members, CMS receives their sociodemographic data from the Social Security Administration, while the states send information for people enrolled in Medicaid, the Children’s Health Insurance Program (CHIP), and health insurance marketplace programs.
Each program has its variation of data standards. The lack of a common health equity data environment will challenge access, integration, and use of the information.
Lastly, there can be implicit bias in health data collection. While developing the HEI, CMS may miss some important data due to possible implicit bias in health data collection and analysis. For example, because there is a limited understanding of how sexual orientation and gender identity (SOGI) can shape an individual’s health, it’s been historically challenging for the CMS to develop standards around SOGI data that would help to understand and address the needs of individuals based on their SOGI.
When Does the HEI Go Into Effect?
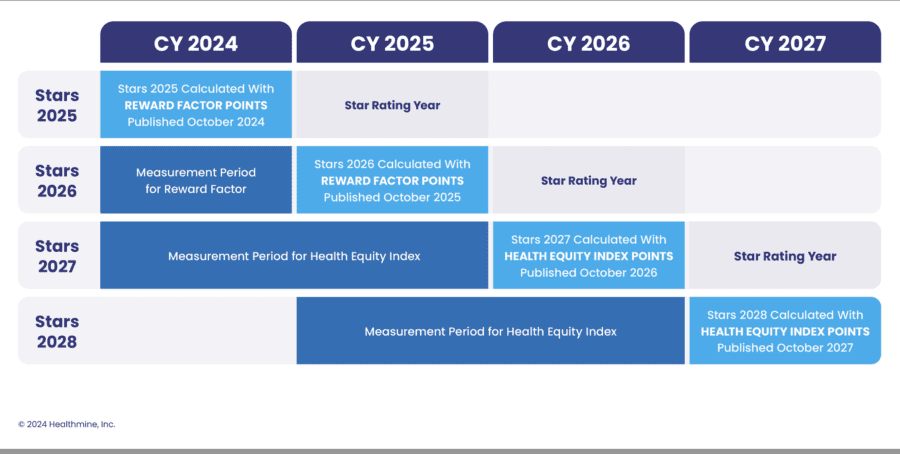
HEI data will be collected during the 2024 and 2025 measurement periods for the 2027 Star Ratings (2028 payment year). All MA organizations are included in this rule, though only plans meeting the minimum threshold of beneficiaries with social risk factors are eligible for rewards.
One immediate opportunity is to enroll and better serve beneficiaries with social risk factors, as current performance will impact Star ratings measured when the initiative takes effect.
Health Equity Index Timeline
Below is a timeline of when the Health Equity Index will start measuring social risk factor data, when it will impact Star Ratings and when CMS will eliminate the current Reward factor.
Health Equity: Areas of Impact
Maintaining (or increasing) Star Ratings is an important strategy in the competitive MA market, as these ratings directly impact plan revenue.
According to a simulation, CMS expects about 2% of contracts to gain one-half Star and 13% of contracts to lose one-half Star as a result of replacing the current system with the Health Equity Index. CMS expects this change to result in program savings of $670 million for the federal government in 2028, driven by a reduction in rebate dollars.
The actual impact of these rule changes on a given contract will depend on many factors, including risk scores, bid-to-benchmark ratios, and the disparities in care between members with and without social risk factors, according to a Milliman report. However, the report recommends that all MA organizations evaluate the impact these changes will have on their contracts and consider adjusting their strategies for the 2024 and 2025 measurement years.
“To succeed under this new structure, Medicare Advantage plans will need to understand their vulnerable populations and deliver targeted, high-impact services to close the gaps that impact health equity,” said Shah.
“In many instances, this means connecting to non-medical home-based partners and tapping into their observations to access really important insights around social, behavioral, and functional health status that really can make a massive impact on outcomes.”

MA Plans are Booming:
How Will You Stay Competitive?
Download our report “Home Benefits Surge in Popularity Among Medicare Advantage Plans” to learn more about leveraging supplemental benefits to increase member satisfaction, retention and STARs.





