In an effort to increase hospital capacity, the Centers for Medicare & Medicaid Services (CMS) launched “unprecedented” steps to provide hospital-level care for patients in their homes.
CMS’s “Acute Hospital Care at Home” program, announced in November, gives hospitals regulatory flexibilities to provide care outside a traditional hospital setting, including in the home. The program is an expansion of its “Hospital Without Walls” initiative launched in March, and is part of a comprehensive effort to increase hospital capacity, maximize resources, and combat COVID-19.
What does it mean?
Hospital-at-home programs provide a higher level of care than traditional home health services, which generally focus on skilled nursing and physical therapy.
Under the CMS program, hospitals apply for a special waiver that allows them to receive inpatient payment for providing acute-level services to Medicare beneficiaries in their homes. The waiver covers 60 acute conditions including asthma, pneumonia, congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD). Currently, 56 systems, 129 hospitals in 30 states have been approved.
Now that there is a financial reimbursement framework in place, health systems are starting to take care-at-home seriously.
There is no deadline for applying. According to CMS, the waiver is only in effect for the duration of the Covid-19 public health emergency.
New care models emerge
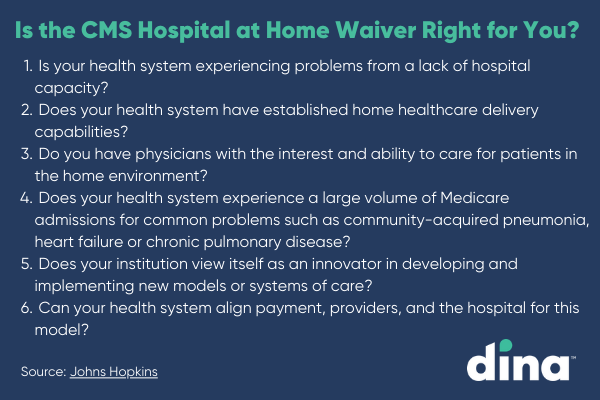
The Acute Hospital Care at Home program builds off the success of early hospital-at-home models pioneered by Johns Hopkins Medicine, Mount Sinai Hospital and others.
The pandemic has spurred adoption of care-at-home models, including the growth of new provider groups like Contessa Health, Medically Home Group, and DispatchHealth, that deliver hospital-level care at home.
“We continue to see a meaningful transition toward home care,” said Dina CEO Ashish V. Shah. “There was a movement prior to Covid to provide more health services to people in their homes and communities, and this has accelerated through the pandemic. We know it’s safer, less expensive, and often produces better health outcomes for patients.”
How does it work?
The following are prerequisites for at-home care under CMS’s “Acute Hospital Care at Home” program:
- Patients can only be cleared for at-home care after being admitted into emergency departments or inpatient hospital settings.
- Patients must be examined by a physician in-person prior to beginning care at home.
- Patients opt into the program and it is up to them whether to receive care in a hospital setting or at home.
The care delivery model includes:
- Extended nursing care to start, then daily nursing visits. Nurses are available 24/7 for urgent or emergent situations.
- Daily physician evaluations with 1+ home visits per day. Physicians are available 24/7 for urgent/emergent situations.
- Two sets of vitals signs obtained daily, in person by clinical team staff.
- Remote monitoring should be consistent with existing hospital policies and standards of care. •Care pathways use illness-specific care maps, clinical outcome evaluations, and specific discharge criteria.
- Diagnostics and treatments at home can include echocardiograms, x-rays, oxygen therapy, intravenous fluids, pharmacy services, and skilled nursing services.
- Hospital trips are required for some procedures like MRIs and endoscopies.
- Once patients are discharged, they are transitioned back to primary care physicians.
Here to stay?
Some stakeholders say they are seeing an acceleration in higher-acuity home care. But many participating hospitals are waiting to see whether CMS, under the Biden administration, will make the conditions of the waiver permanent. Separately, the proposed $2 trillion-plus American Jobs Act includes $400 billion for home care, a move in the right direction.
“This is clearly a sign that CMS is taking care-at-home seriously,” said Shah. “Now that there is a financial reimbursement framework in place, healthcare systems are starting to take it seriously, too. My hope is that this program remains in place after the pandemic subsides. It just makes sense to continue to fund care-at-home.”
Want more healthcare-at-home news? Download our recent webinar with Becker’s Hospital Review: The Rise of Home-Based Care: How Jefferson Health is Engaging Patients at Scale.